Abstract
Purpose
To evaluate the psychological consequences among family members given the option to be present during the CPR of a relative, compared with those not routinely offered the option.
Methods
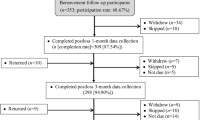
Prospective, cluster-randomized, controlled trial involving 15 prehospital emergency medical services units in France, comparing systematic offer for a relative to witness CPR with the traditional practice among 570 family members. Main outcome measure was 1-year assessment included proportion suffering post-traumatic stress disorder (PTSD), anxiety and depression symptoms, and/or complicated grief.
Results
Among the 570 family members [intention to treat (ITT) population], 408 (72 %) were evaluated at 1 year. In the ITT population (N = 570), family members had PTSD-related symptoms significantly more frequently in the control group than in the intervention group [adjusted odds ratio, 1.8; 95 % confidence interval (CI) 1.1–3.0; P = 0.02] as did family members to whom physicians did not propose witnessing CPR [adjusted odds ratio, 1.7; 95 % CI 1.1–2.6; P = 0.02]. In the observed cases population (N = 408), the proportion of family members experiencing a major depressive episode was significantly higher in the control group (31 vs. 23 %; P = 0.02) and among family members to whom physicians did not propose the opportunity to witness CPR (31 vs. 24 %; P = 0.03). The presence of complicated grief was significantly greater in the control group (36 vs. 21 %; P = 0.005) and among family members to whom physicians did not propose the opportunity to witness resuscitation (37 vs. 23 %; P = 0.003).
Conclusions
At 1 year after the event, psychological benefits persist for those family members offered the possibility to witness the CPR of a relative in cardiac arrest.

Similar content being viewed by others
References
Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, Fassier T, Galliot R, Garrouste-Orgeas M, Goulenok C, Goldgran-Toledano D, Hayon J, Jourdain M, Kaidomar M, Laplace C, Larche J, Liotier J, Papazian L, Poisson C, Reignier J, Saidi F, Schlemmer B (2005) Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med 171:987–994
Bourgeois ML (2006) Qualitatives and quantitative methods in grief studies. Ann Med Psychol (Paris) 164:278–291
Prigerson HG, Bierhals AJ, Kasl SV, Reynolds CF 3rd, Shear MK, Day N, Beery LC, Newsom JT, Jacobs S (1997) Traumatic grief as a risk factor for mental and physical morbidity. Am J Psychiatry 154:616–623
Prigerson HG, Frank E, Kasl SV, Reynolds CF, Anderson B, Zubenko GS, Houck PR, Georges CJ, Kupfer DJ (1995) Complicated grief and bereavement-related depression as distinct disorders: preliminary empirical validation in elderly bereaved spouses. Am J Psychiatry 152:22–30
Ricard-Hibon A, Chollet C, Saada S, Loridant B, Marty J (1999) A quality control program for acute pain management in prehospital critical care medicine. Ann Emerg Med 34:738–744
Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, Barnoud D, Bleichner G, Bruel C, Choukroun G, Curtis JR, Fieux F, Galliot R, Garrouste-Orgeas M, Georges H, Goldgran-Toledano D, Jourdain M, Loubert G, Reignier J, Saidi F, Souweine B, Vincent F, Barnes NK, Pochard F, Schlemmer B, Azoulay E (2007) A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 356:469–478
Robinson SM, Mackenzie-Ross S, Campbell Hewson GL, Egleston CV, Prevost AT (1998) Psychological effect of witnessed resuscitation on bereaved relatives. Lancet 352:614–617
Doyle CJ, Post H, Burney RE, Maino J, Keefe M, Rhee KJ (1987) Family participation during resuscitation: an option. Ann Emerg Med 16:673–675
Morrison LJ, Kierzek G, Diekema DS, Sayre MR, Silvers SM, Idris AH, Mancini ME (2010) Part 3: ethics: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 122:S665–S675
Downar J, Kritek PA (2013) Family presence during cardiac resuscitation. N Engl J Med 368:1060–1062
McClenathan BM, Torrington KG, Uyehara CFT (2002) Family member presence during cardiopulmonary resuscitation: a survey of US and international critical care professionals. Chest 122:2204–2211
Jabre P, Belpomme V, Azoulay E, Jacob L, Bertrand L, Lapostolle F, Tazarourte K, Bouilleau G, Pinaud V, Broche C, Normand D, Baubet T, Ricard-Hibon A, Istria J, Beltramini A, Alheritiere A, Assez N, Nace L, Vivien B, Turi L, Launay S, Desmaizieres M, Borron SW, Vicaut E, Adnet F (2013) Family presence during cardiopulmonary resuscitation. N Engl J Med 368:1008–1018
Meyers TA, Eichhorn DJ, Guzzetta CE, Clark AP, Klein JD, Taliaferro E, Calvin A (2000) Family presence during invasive procedures and resuscitation. Am J Nurs 100:32–42 quiz 43
Mian P, Warchal S, Whitney S, Fitzmaurice J, Tancredi D (2007) Impact of a multifaceted intervention on nurses’ and physicians’ attitudes and behaviors toward family presence during resuscitation. Crit Care Nurse 27:52–61
Horowitz M, Wilner M, Alvarez W (1979) Impact of event scale: a measure of subjective stress. Psychosomatic Med 41:209–218
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Prigerson HG, Maciejewski PK, Reynolds CF 3rd, Bierhals AJ, Newsom JT, Fasiczka A, Frank E, Doman J, Miller M (1995) Inventory of complicated grief: a scale to measure maladaptive symptoms of loss. Psychiatry Res 59:65–79
Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar G (1998) The Mini International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview. J Clin Psychiatry 59(Suppl 20):22–33
Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, Grassin M, Zittoun R, le Gall JR, Dhainaut JF, Schlemmer B (2001) Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med 29:1893–1897
Bourgeois ML (2004) Les deuils traumatiques. Stress et Trauma 4:241–248
Sheehan DV, Lecrubier Y, Harnett-Sheehan K, Janavs J, Weiller E, Bonora LI, Keskiner A, Schinka J, Knapp E, Sheehan MF, Dunbar GC (1997) Reliability and validity of the MINI international neuropsychiatric interview (M.I.N.I.): according to the SCID-P. Eur Psychiatry 12:232–241
Compton S, Levy P, Griffin M, Waselewsky D, Mango L, Zalenski R (2011) Family-witnessed resuscitation: bereavement outcomes in an urban environment. J Pall Med 14:715–721
Rubin DB (1987) Multiple imputation for nonresponse in surveys. Wiley, New York
Belpomme V, Adnet F, Mazariegos I, Beardmore M, Duchateau FX, Mantz J, Ricard-Hibon A (2013) Family-witnessed resuscitation: nationwide survey of 337 out-of-hospital emergency teams in France. Emerg Med J 30:1038–1042
Colbert JA, Adler JN (2013) Clinical decisions. Family presence during cardiopulmonary resuscitation—polling results. N Engl J Med 368:e38
Antonelli M, Bonten M, Chastre J, Citerio G, Conti G, Curtis JR, De Backer D, Hedenstierna G, Joannidis M, Macrae D, Mancebo J, Maggiore SM, Mebazaa A, Preiser JC, Rocco P, Timsit JF, Wernerman J, Zhang H (2012) Year in review in intensive care medicine 2011: I. Nephrology, epidemiology, nutrition and therapeutics, neurology, ethical and legal issues, experimentals. Intensive Care Med 38:192–209
Lind R, Lorem GF, Nortvedt P, Hevroy O (2011) Family members’ experiences of “wait and see” as a communication strategy in end-of-life decisions. Intensive Care Med 37:1143–1150
Latham AE, Prigerson HG (2004) Suicidality and bereavement: complicated grief as psychiatric disorder presenting greatest risk for suicidality. Suicide Life Threaten Behav 34:350–362
Meert KL, Donaldson AE, Newth CJ, Harrison R, Berger J, Zimmerman J, Anand KJ, Carcillo J, Dean JM, Willson DF, Nicholson C, Shear K (2010) Complicated grief and associated risk factors among parents following a child’s death in the pediatric intensive care unit. Archiv Pediatr Adolesc Med 164:1045–1051
Chen JH, Bierhals AJ, Prigerson HG, Kasl SV, Mazure CM, Jacobs S (1999) Gender differences in the effects of bereavement-related psychological distress in health outcomes. Psychol Med 29:367–380
Boelen PA, Prigerson HG (2007) The influence of symptoms of prolonged grief disorder, depression, and anxiety on quality of life among bereaved adults: a prospective study. Eur Archiv Psychiatry Clin Neurosci 257:444–452
Acknowledgments
Supported by the Programme Hospitalier de Recherche Clinique 2008 of the French Ministry of Health and by the Research Delegation of the Assistance Publique – Hopitaux de Paris (Aurélie Guimfack and Christine Lanau). We are indebted to Martine Tanke, who monitored the ongoing results of the trial; to the physicians, nurses, and ambulance attendants of each center for their valuable cooperation with the study; to Malika Chafai for her secretarial assistance. This study was funded solely by the Programme Hospitalier de Recherche Clinique 2008 of the French Ministry of Health.
Conflicts of interest
No author has a conflict of interest with regard to this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: The long-term benefits on post-traumatic stress disorder and depression to being offered the possibility of witnessing resuscitation are still present at 1 year. The incidence of traumatic grief is diminished when a family member is offered the possibility of witnessing CPR.
Trial registration: ClinicalTrials.gov number, NCT01009606.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jabre, P., Tazarourte, K., Azoulay, E. et al. Offering the opportunity for family to be present during cardiopulmonary resuscitation: 1-year assessment. Intensive Care Med 40, 981–987 (2014). https://doi.org/10.1007/s00134-014-3337-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3337-1